Diagnosis
To diagnose peripheral artery disease (PAD), a healthcare professional examines you. You are usually asked questions about your symptoms and medical history.
If you have peripheral artery disease, the pulse in the affected area may be weak or missing.
Tests
Tests to diagnose peripheral artery disease (PAD) or check for conditions that cause it may include:
- Blood tests. Blood tests are done to check for things that increase the risk of PAD, such as high cholesterol and high blood sugar.
- Ankle-brachial index (ABI). This is a common test used to diagnose PAD. It compares the blood pressure in the ankle with the blood pressure in the arm. You may be asked to walk on a treadmill. Blood pressure readings may be taken before and right after exercising to check the arteries during walking.
- Ultrasound of the legs or feet. Sound waves create pictures of how blood moves through the blood vessels of the legs or feet. Doppler ultrasound is a special type of ultrasound used to spot blocked or narrowed arteries.
- Angiography. This test uses imaging tests and a dye to look for blockages in the arteries. The dye is given through a blood vessel. It helps the arteries show up more clearly on the test images.
More Information
Treatment
The goals of treatment for peripheral artery disease (PAD) are:
- Manage symptoms, such as leg pain, so exercise is comfortable.
- Improve artery health to reduce the risk of heart attack, stroke and other complications.
Treatment for peripheral artery disease may include:
- Lifestyle changes.
- Medicine.
- Surgery.
Lifestyle changes can help improve symptoms, especially if you have early peripheral artery disease. Such changes include:
- Don't smoke or use tobacco.
- Get regular exercise.
- Eat a healthy diet.
Medications
If you have symptoms or complications of peripheral artery disease (PAD), you may need medicines.
Medicine to treat peripheral artery disease may include:
- Statins. These are medicines to lower "bad" cholesterol. They help reduce plaque buildup in the arteries. The drugs also lower the risk of heart attacks and strokes.
- Blood pressure medicines. Uncontrolled high blood pressure can make arteries stiff and hard. This can slow the flow of blood. If you have high blood pressure, your healthcare professional may suggest medicines to control it. Ask your healthcare team what your blood pressure should be.
- Diabetes medicine. Diabetes makes you more likely to get PAD. Talk with your healthcare team about your blood sugar goals and how to reach them.
- Medicines to prevent blood clots. Reduced blood flow in PAD can cause blood clots. Aspirin or another medicine, such as clopidogrel (Plavix), may be used to prevent blood clotting.
- Leg pain medicine. A medicine called cilostazol can be used to treat leg pain in people with peripheral artery disease. The medicine increases blood flow to the area.
Surgeries or other procedures
Graft bypass
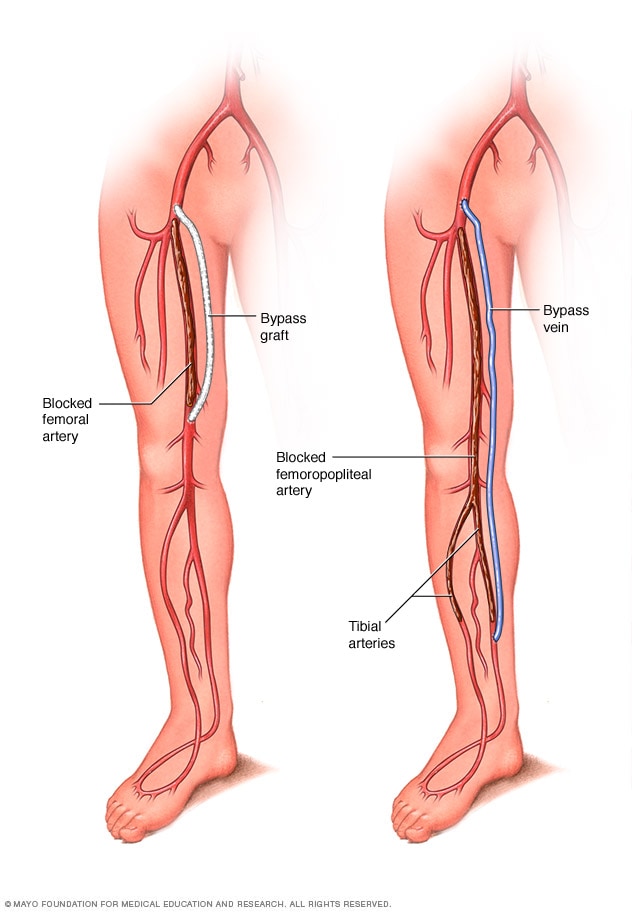
Graft bypass
A graft is used to redirect blood flow around a blocked or narrowed artery. A graft can be a blood vessel from another part of the body or a synthetic substitute.
Sometimes, a surgery or procedure is needed to treat peripheral artery disease (PAD) or its symptoms.
- Thrombolytic therapy. If a blood clot is blocking an artery, medicine may be given directly into the affected artery to dissolve the clot.
- Angioplasty and stent placement. If a narrowed artery is causing PAD leg pain, this treatment may help. A tiny balloon on a tube, called a catheter, is placed in the artery. The balloon inflates, which makes the artery wider. This improves blood flow. A small wire mesh tube, called a stent, may be placed in the artery to keep the artery open.
- Bypass surgery. This surgery creates a new path for blood to flow around a blocked or partially blocked artery. A surgeon takes a healthy blood vessel from another part of the body. The vessel is connected below the blocked artery. The new pathway improves blood flow to the muscle.
Lifestyle and home remedies
There are things you can do to help manage peripheral artery disease (PAD). Try these tips to manage PAD and stop symptoms from getting worse:
- Don't smoke or use tobacco. Smoking damages the arteries. It increases the risk of peripheral artery disease. If you have PAD, smoking can make the condition worse. If you smoke and need help quitting, ask your care team about methods that can help.
-
Get regular exercise. Regular exercise is an important part of peripheral artery disease (PAD) treatment. Exercise helps improve blood flow to the arms and legs. So it can improve symptoms of PAD.
Usually, healthcare professionals recommend supervised exercise therapy for people with PAD. It's a program of exercise and education. It can help increase the distance you can walk pain-free.
- Eat nutritious foods. Choose plenty of fruits, vegetables and whole grains. Reduce sugar, salt and saturated fats.
- Check medicine labels. Products that contain pseudoephedrine (Advil Cold and Sinus, Claritin D, others) are often used to treat a stuffy nose due to allergies or colds. But this ingredient tightens blood vessels. It may increase PAD symptoms.
- Check leg position. Try sleeping with the head of the bed raised a few inches. Keeping the legs below the level of the heart usually reduces pain. Some people find that hanging their legs over the edge of the bed or walking may temporarily reduce leg pain.
Foot care
It's important to take good care of your feet. PAD can make it harder for cuts and sores on the lower legs and feet to heal. This is especially true if you have PAD and diabetes.
Here is how to properly care for your feet:
- Wash your feet every day. Dry them completely.
- Use moisturizer on the feet to prevent cracks that can lead to infection. But don't moisturize between the toes. This can help fungus grow.
- Wear thick, dry socks and well-fitting shoes.
- Quickly treat any fungal infections of the feet, such as athlete's foot.
- Take care when trimming your toenails.
- Check your feet daily for cuts, sores or other injuries. See a healthcare professional if you find any.
- Have a foot doctor, called a podiatrist, treat bunions, corns or calluses.
Preparing for your appointment
If you have leg pain or other symptoms of peripheral artery disease (PAD), make an appointment for a health checkup. You may need to see a doctor trained in blood vessel diseases, called a vascular specialist.
Here's some information to help you get ready for your appointment.
What you can do
- Learn what you need to do before your appointment. Ask if there's anything you need to do in advance, such as restrict your diet. For example, you may be told not to eat or drink for a few hours before a cholesterol test.
- Write down any symptoms you're having, including any that may seem unrelated to peripheral artery disease.
- Write down your medical information, including other conditions you have and any family history of heart disease.
- Bring a list of medicines with you to your appointment. Include supplements and any medicines bought without a prescription. Also include dosages.
- Ask a family member or friend to go with you to the appointment, if possible. An extra person can help you remember details from the appointment.
- Write down questions to ask your healthcare team.
For peripheral artery disease (PAD), some basic questions to ask your healthcare professional are:
- What's the most likely cause of my symptoms?
- Are there other possible causes?
- What types of tests do I need? Do these tests require any special preparation?
- Is peripheral artery disease temporary or long lasting?
- What treatments are available? Which do you recommend?
- What are the side effects of the treatment you are suggesting?
- Are there any options to the treatment that you're suggesting?
- What can I do on my own that might help me get better?
- I have other health conditions. How can I best manage these conditions together?
- Are there any brochures or other printed material that I can take home with me? What websites do you recommend?
Don't hesitate to ask any other questions.
What to expect from your doctor
A healthcare professional who sees you for peripheral artery disease (PAD) might ask:
- When did the symptoms start?
- Do you always have symptoms, or do they come and go?
- How bad are your symptoms?
- Do your symptoms get worse when you exercise?
- Do your symptoms get better when you're resting?
- Did you or do you smoke or use tobacco? If yes, how often?
What you can do in the meantime
If you smoke, quit. Smoking increases the risk of peripheral artery disease (PAD) and related conditions such as stroke and heart attack. Smoking also can make existing PAD worse. If you need help quitting, ask your care team for methods that can help.
Eating less saturated fat and adding more fruits and vegetables to your diet are other things you can do to help prevent or manage PAD.
Aug. 09, 2024